News & Updates — President’s Update
It’s the rare person who won’t admit to feeling some pandemic fatigue these days — from the clinicians still treating COVID-19 patients to the parents juggling work, child care, and virtual school to the many of us missing family and friends. But in the midst of today’s challenges, I have been gratified and humbled to see how our grantees are finding innovative ways to carry on their work, despite the necessary restrictions of the pandemic.
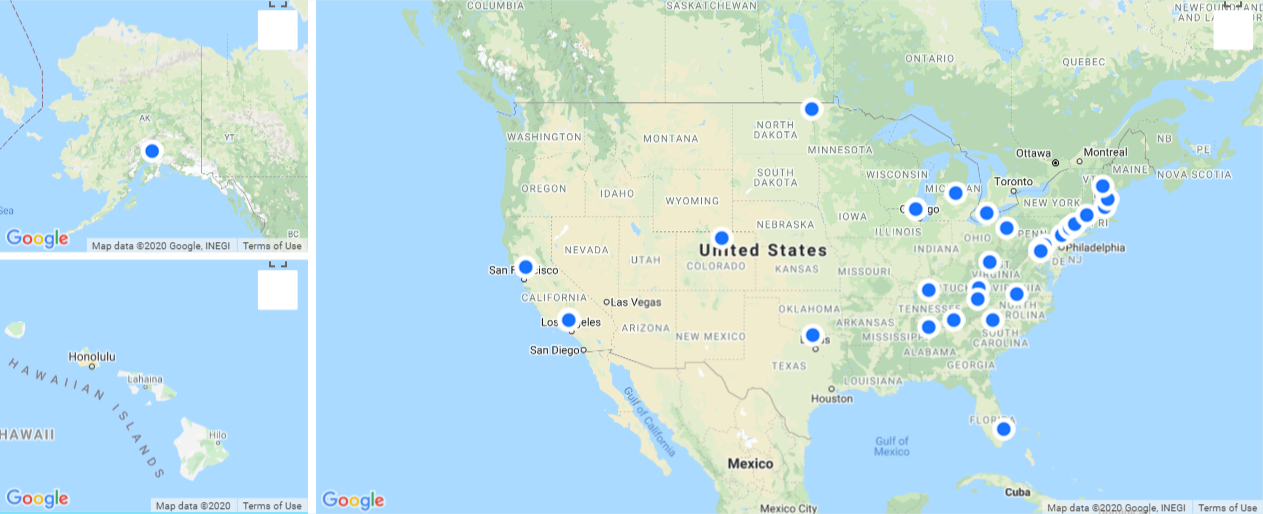
In mid-March as the pandemic was just hitting New York City, we had just awarded our first round of grants to 19 organizations that are expanding access to opioid use disorder (OUD) treatment for vulnerable groups, including pregnant women, people experiencing homelessness, and those just released from jails or prisons who are at high risk of relapse and overdose deaths.
Given the timing, I would not have been surprised if some of our grantees told us they couldn’t launch the projects as they had planned. But that wasn’t the case. When social restricting rules hit their regions, many of our grantees pivoted quickly, taking advantage of relaxed telehealth rules to stand up telemedicine models and expand the reach of their clinics, initiating medication for opioid use disorder (MOUD) treatment, and staying connected with patients. Other grantees developed innovative ways to initiate their projects safely, including leveraging digital tools to strengthen relationships with clients and gain input from key stakeholders. At the same time, we saw those involved in data collection and/or policy-related projects add questions that will enable us to learn from the natural experiments playing out during the pandemic.
Not one grantee told us they couldn’t carry on their work; to the contrary, all have been able to move forward in their efforts to expand access to OUD treatment and recovery services. I’ll share just a few examples of the many milestones they’ve hit so far:
- Although emergency department (ED) physicians see more OUD patients than other specialists, few initiate MOUD treatment. To change that, ED physicians at Massachusetts General Hospital are leading Get Waivered, a national campaign to encourage ED clinicians to pursue the federal waivers needed to prescribe buprenorphine for MOUD. While before the pandemic, their in-person waiver training courses had 20 to 30 clinicians at a time, nearly 1,200 clinicians registered for the first Get Waivered virtual Zoom training in May — and more than 800 completed the course.
- Once clinicians get waivered, they still need help in delivering OUD treatment. The American College of Emergency Physicians is using quality improvement and performance benchmarking to promote best practices for treating OUD in EDs. Clinicians from 355 EDs around the country signed up in June to participate in this ongoing effort.
- Hub-and-spoke systems are one strategy states have used to expand access to MOUD and the continuum of care for OUD patients. From hubs at two addiction treatment programs in North Carolina, UNC Health Sciences at Mountain Area Health Education Center (MAHEC) is providing training and care management support to providers in community health centers and local health department clinics — the spokes— who are willing to offer treatment for OUD. Despite the pandemic, MAHEC has already been able to engage 52 health center and health departments clinic sites in 28 counties, across the state.
Over the course of the summer, we awarded grants that build on our efforts to ensure access to treatment and recovery services during the pandemic and leverage opportunities to inform future policy and practice. Some of the grants we made as part of our COVID-19 response help frontline providers of recovery support services sustain their work, for example by shifting from in-person to virtual platforms, creating mobile apps that offer evidence-based OUD interventions, or implementing telehealth treatment services at free clinics.
Emerging evidence suggests that opioid use and overdoses have been increasing during the pandemic, and our grantees are saying there’s overwhelming demand for services. Reports from our most recent grantees include:
- The Addiction Policy Forum is offering individuals involved with drug courts and diversion programs, many of whom are unable to access in-person treatment programs, free access to their Connections mobile app, which offers on-demand treatment and supports from addiction specialists and peers. Demand for 1,000 available spots currently outpaces supply.
- As part of the health system’s strategy to reduce OUD in its Appalachian region, Ballad Health has been giving people in recovery the opportunity to help others. The health system received 90 applications for its first 12 slots to train as peer recovery specialists.
- Similarly, in Cleveland, Ohio, the Hispanic Urban Minority Alcoholism and Drug Abuse Outreach Program received an overwhelming response to its call for peer recovery specialists who can offer culturally tailored services, in both Spanish and English.
Sadly, there is every indication that the need for these services and further systems improvements remains and will grow. I’m so impressed and gratified to see the innovative ways in which our grantees are leading this work, finding ways to carry on, and helping those affected by the OUD crisis.