News & Updates — President’s Update
President’s Update, Apr. ’23: Learning from Our Grantees as We Launch New Programs
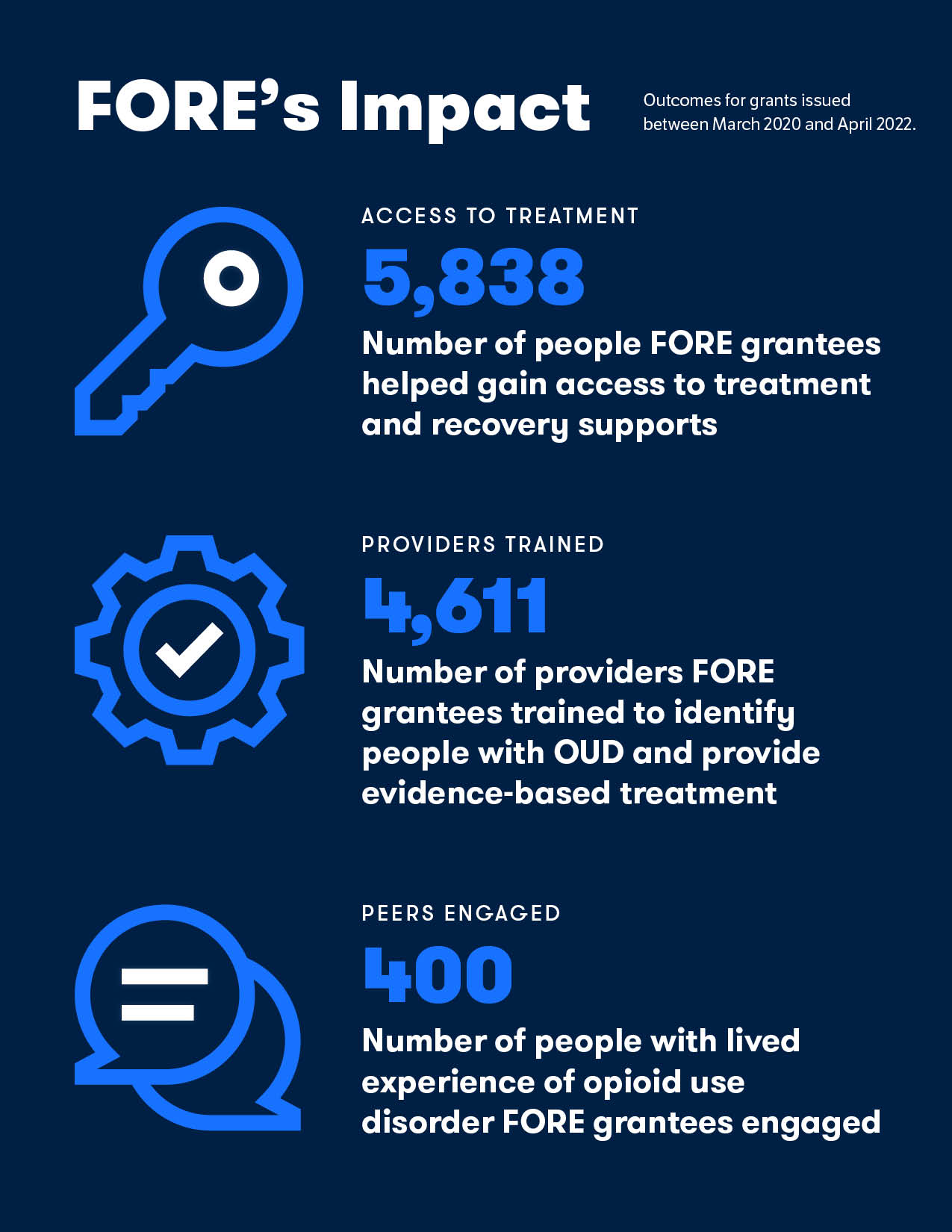
April 25, 2023As I read through FORE’s latest Annual Report, I’m struck by the real-world impacts we’re making and insights we’re gaining by working with a growing cadre of impressive grantees. In addition to launching innovative programs that have expanded access to treatment and recovery supports for people with opioid use disorder (OUD), our grantees have documented the effects of policy changes on patients and providers and identified opportunities to intervene.
Based in part on those insights, we launched two new programs in 2022. One focuses on strategies for preventing OUD and other substance use disorders. We’re supporting organizations working to improve and expand evidence-based prevention programs for children and families and mitigate the effects of adverse childhood experiences (ACEs), including parental substance use, abuse, or neglect, in an effort to disrupt intergenerational cycles of addiction. The second — our innovation program — supports novel approaches to perennial challenges, including the stigma that many people with OUD encounter when they seek help from health professionals, clergy, and others and the lack of access to timely and actionable data about the evolving crisis.
We’ve also just launched a program that supports community-based organizations working to reduce OUD and overdose deaths. In reviewing the 428 proposals we received, we heard about the pressing needs of small organizations to build their staff, technology, and outreach efforts. We’re providing 15 community-based organizations with operational support to help them increase their abilities to reach groups deeply affected by the opioid crisis, including Black, Hispanic, and LGBTQ+ people as well as those living in rural areas and those being released from jails or prisons.
As we move forward with these new programs, we also continue to reflect on what we have learned from our first grantees. Here are a handful of those lessons.
COVID-19 Flexibilities Promoted Continuity of Care But Did Not Expand Access
To preserve access to medications for OUD (MOUD) during the pandemic, federal regulators relaxed the guidelines governing treatment.
In a new issue brief, we report findings from five grantees who interviewed nearly 500 patients taking MOUD and nearly 400 providers to see how these treatment flexibilities — enabling take-home doses of methadone and permitting buprenorphine induction via telehealth, among others — affected them. They found that there were few negative, unintended consequences: providers did not report substantial increases in drug diversion, overdoses, or patients dropping out of treatment.
Still, not all providers adopted these voluntary changes and not all patients benefited. Beth E. Meyerson, PhD, MDiv, and colleagues at the University of Arizona found that patients in Arizona did not benefit from telehealth or allowances for take-home doses of methadone because the state didn’t mandate that providers implement them. Some patients interviewed for the study, published in PLOS ONE, said they were required to come to a clinic to attend video appointments with providers who stayed offsite. And while about half of patients received some take-home doses of methadone, none said they received the federally allowed 14- or 28-day supplies.
Another grantee, Bradley D. Stein, MD, PhD, and colleagues at RAND Corp., found in a study published in the Journal of General Internal Medicine that while buprenorphine prescribing held steady in 2020 compared to 2019, the numbers of people entering and leaving treatment were lower than expected. This suggests the temporary relaxation of rules and enhancements in Medicaid coverage may have helped some patients stay in treatment but did not facilitate access for new patients.
Missed Opportunities to Prevent and Respond to Substance Use Among Youth
Research from Lisa Clemans-Cope, PhD, Victoria Lynch, MS, and colleagues from the Urban Institute highlights opportunities for health care providers to identify more youth coping with OUD and other substance use disorders and offer them treatment. Using Medicaid claims data, they found more than one-quarter of youth with unhealthy opioid use and a third of youth with OUD were receiving mental health care for depression and anxiety and other conditions — a point of contact that could be leveraged to address substance use as well. They also found that although youth interact with health professionals at high rates, many aren’t screened or treated for substance use.
The Urban Institute researchers also found that about half of youth with a SUD or other behavioral health diagnosis received services in an emergency department, compared with about 20 percent of youth without such diagnoses. Most youth with behavioral health diagnoses did not get any health services in schools.
A FORE-supported workshop conducted by the National Academies for Sciences, Engineering, and Medicine explored ways pediatricians and other primary care providers can help prevent substance use disorders among adolescents. The resulting report and interactive website provide evidence of what works and suggest ways for providers to initiate conversations with adolescents about substance use and partner with schools and others to connect families to prevention programs.
A number of FORE’s prevention projects focus on bringing more capacity to schools, including a grant that’s leveraging the University of New Mexico’s Project ECHO telehealth platform to train nurses, counselors, and teachers in schools across the state to identify and mitigate risk factors that can fuel opioid use among children and adolescents.
Looking Ahead
We’re learning from our grantees that while policy changes are critical to expanding access to OUD prevention, treatment, and recovery, they are not sufficient. We also need new approaches to training, innovative models of delivery and payment, and most important, the insights of people with lived experience of OUD. I’m confident that we will continue to make headway in these areas and others as we work to bring solutions to the evolving opioid crisis.
Karen A. Scott, MD, MPH
President