News & Updates — Grantee Spotlight
Grantee Spotlight: Educating Providers About the Consequences of Child Welfare Reporting
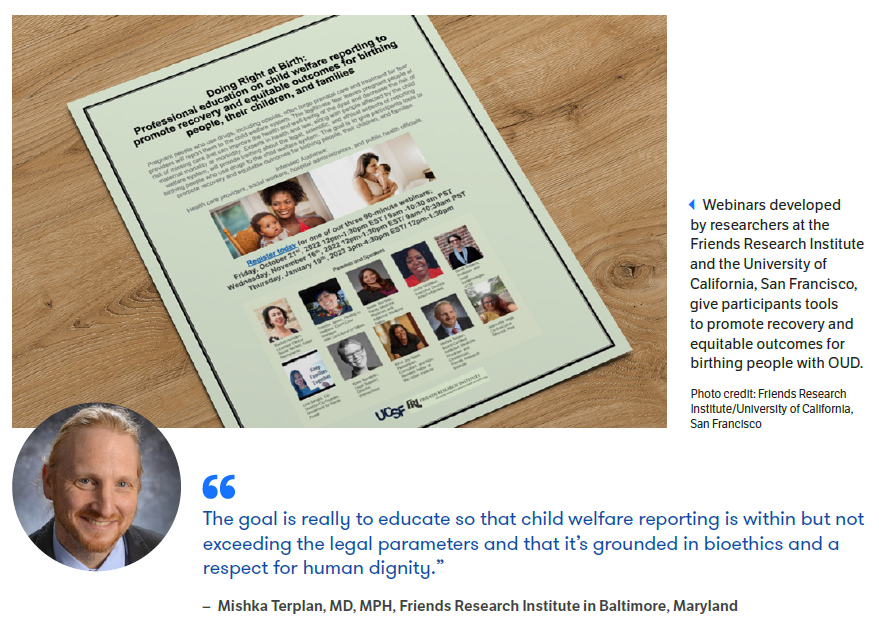
June 29, 2023Fear of being reported to the child welfare system can prevent pregnant people with opioid use disorder (OUD) from seeking either prenatal care or substance use treatment. Widespread stigma against pregnant people who use substances and racism play outsized roles in reporting decisions, which can lead to a child’s placement in foster care or the termination of parental rights. To help clinicians, hospital administrators, and the staff of public health agencies understand the consequences of reporting and make ethically informed decisions, FORE grantees are developing, implementing, and evaluating an array of training tools. FORE spoke to Sarah Roberts, DrPH, from the University of California, San Francisco, and Mishka Terplan, MD, MPH, from the Friends Research Institute — a nonprofit that conducts research on substance use and mental illness — about the project and the changes they’d like to see to ensure more pregnant people with OUD receive the supports they need.
Your project aims to educate physicians, nurses, social workers, and others about the legal, scientific, and ethical aspects of child welfare reporting. What was the impetus?
Terplan: Over the last decade, there’s been a dramatic increase in the use of urine drug testing in hospitals as well as the number of infants reported to the child welfare system (CWS) due to parental substance use. And yet, it’s rare to find a provider who knows much about the CWS. Clinicians and hospital staff tend to make reports reflexively, thinking that doing so will connect people to services. They’re often unaware of negative consequences of reporting, including the impact of family separation on early childhood development and the association between child removals and parental return to use, overdose, and death. Our goal is to ensure that child welfare reporting is done in a way that is ethically sound, respectful, grounded in evidence, and within but not exceeding legal requirements.
Indiscriminate as well as discriminatory drug testing is also a factor in child welfare reporting. A recent study by Roberts, Terplan, and colleagues found Black people who delivered babies at one Pennsylvania health system were more likely to be tested for drug use than white people and less likely to test positive.
What does the training cover?
Roberts: We’ve developed the content in partnership with a community advisory board that includes practicing clinicians, legal experts, and people whose lives have been impacted by the child welfare system. It covers a lot of ground, including the evidence of widespread racial disparities in the use of urine drug testing and CWS reporting, as well as research on the health effects and developmental consequences of CWS involvement. We also provide people with tools to shift their hospital policies regarding drug testing and child welfare reporting. Our community advisory board members were already leading efforts to move health professionals from an approach of mandatory reporting to mandatory supporting and this project amplifies those efforts. It’s a big shift.

Who are you hoping to reach and what do you think will be most persuasive?
Roberts: We want to reach all hospital staff who play a role in reporting decisions, including social workers, nurses, pediatricians, family medicine doctors, psychiatrists, and others. We’re hoping the combination of data and the personal stories of people whose lives have been negatively affected by the CWS will motivate people to rethink their approach. Often people are worried about what will happen if they don’t make a report. They think something is going to happen to the baby and they will be responsible. They may make a report to relieve their own anxiety, without realizing that it creates an immense amount of trauma for families and doesn’t necessarily lead to treatment for substance use disorder or supports for families. We want to give people a more rational framework to use to evaluate their decision to drug test and report.
What would an ethical approach look like?
Terplan: A more ethical approach is to stop what we call the “test and report” chain. Urine drug tests should not be used except in cases where they are necessary to inform a clinical decision. They are not parenting tests and they should not be used to inform CWS reporting decisions. Drug use in pregnancy is evidence of an untreated medical condition and not de facto child abuse. Therefore, CWS reporting should be limited to only the cases where the law requires such reporting and should not exceed these requirements. Because child welfare is not a service agency, health professionals should work to identify community resources to which they can connect pregnant and birthing people who use drugs and provide evidence-based and trauma-informed treatment to people with OUD.

What sorts of supports do expectant parents and families need when substance use issues are identified? To what extent are these available either in hospitals or after discharge?
Terplan: The best guide to what expectant parents need are the parents themselves. They may request support accessing treatment, housing, or transportation or something altogether different. From the provider perspective, the best we can do is to treat the people we serve with the dignity and respect they deserve. Specifically, hospitals should be able to screen and diagnose addiction and, for those with a use disorder, initiate treatment and provide referrals if needed to continuing care. Postpartum is a critical period of treatment attrition, due in part to changes in insurance status and the realities of infant care. Providing continuing support through postpartum may require marshalling a variety of resources including early head start programs and the services of doulas and peer recovery workers.
How are you assessing the effectiveness of the training?
Terplan: We’ve been collecting real-time feedback during webinars. We’ve also been conducting an evaluation to assess whether the training reduced stigma, changed attitudes, and changed behaviors with respect to CWS reporting. Preliminary findings suggest shifts in the hoped-for direction, which reinforces that our approach to the webinars is on the right track.
You’re also training a cadre of health professionals to act as champions for policy reforms. What do you hope they will accomplish?
Roberts: We know there are a lot of professionals who share these critiques of the child welfare system but don’t know what to do. The webinars and other training tools we are developing (e.g., a self-paced video course) will be broadly available and we hope that they motivate people to shift their own behavior. To help lead change, though, and change some of the policies and protocols that constrain health professionals’ behavior, we’ve recruited 16 physicians, social workers, and nurses to be part of the inaugural Doing Right at Birth cohort of champions. Cohort members are from a range of institutions, representing all geographic areas of the U.S. Our expectation is that they will spur and support changes in reporting practices and policies in their own institutions, communities, and states. Within a hospital, they might work to change hospital test and report policies. Or they might advise states on how to ensure that a state’s application of federal Child Abuse Prevention and Treatment Act guidelines is done in the least restrictive way.
The Doing Right at Birth team is training 16 health care professionals to spur and support changes in child welfare reporting practices and policies in their own institutions, communities, and states. These champions will also support one another in overcoming shared challenges.